#H. Pylori, #Bacteria #Game #Players #BioFlim # Candida Albicans #Treatment for Fungal protection homes
The Game of LPS and H. Pylori, Candida
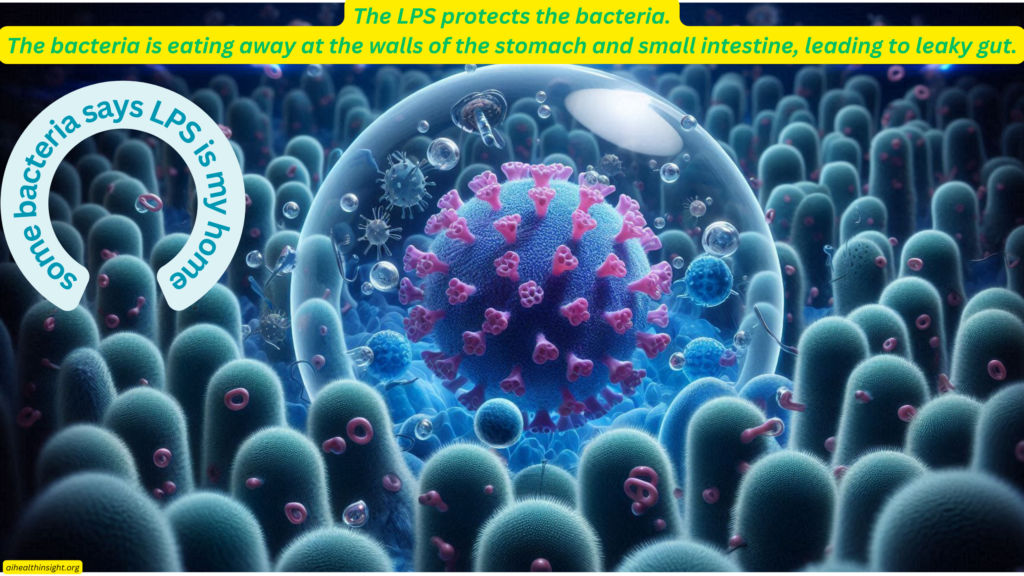
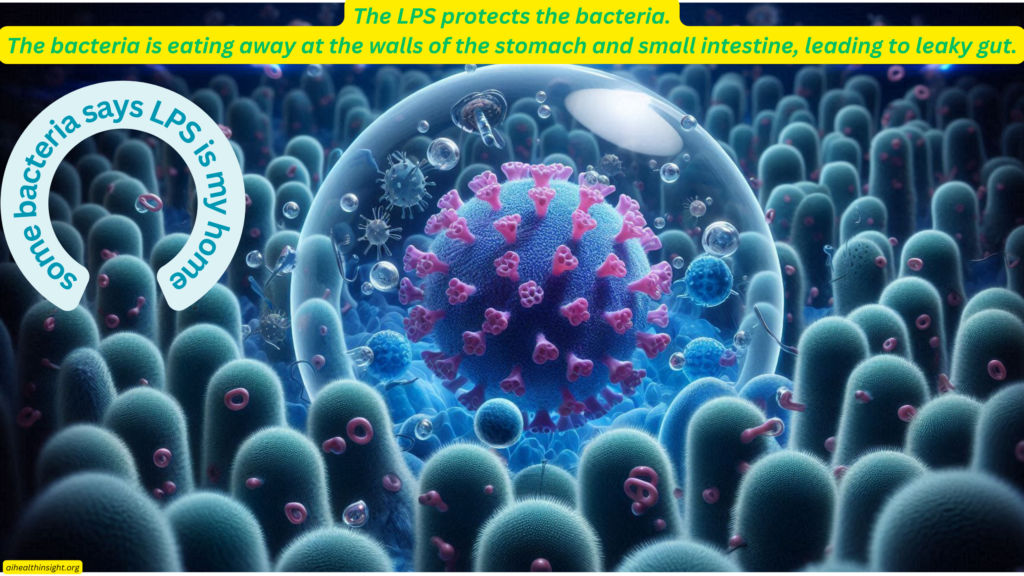
Dealing with lipopolysaccharides (LPS) can be a long and challenging process. For years, you’ve been unknowingly providing glucose and other nutrients to bacteria like H. pylori and E. coli. These bacteria have utilized these substrates (monosaccharides, fatty acids, and proteins) to create their own protective shield—the formidable LPS. (Home or protective shield of these gram negative guys)

Now, these bacteria are using LPS to trigger your immune system, causing it to respond aggressively. This results in inflammation and damage to your gut lining, creating microscopic holes that allow the bacteria and their toxins to infiltrate further. This battle, unfortunately, makes it feel like your immune system is attacking you rather than protecting you.
The Vicious Cycle
The immune response to LPS can actually aid the bacteria in causing more damage. The immune system’s attack on the LPS can inadvertently break down the walls of your stomach and small intestine more effectively than the bacteria alone could. The bacteria simply poke at the immune system, provoking a response that leads to more harm to your intestinal walls. This creates a vicious cycle where the bacteria thrive and continue to cause damage.
Winning the Battle Against LPS and H. pylori
To break this cycle, it’s essential to address both the bacteria and their protective LPS shield. Here’s a protocol to consider:
- Antibiotics: Whether using prescribed antibiotics ( GP will prescribe after testing) or herbal alternatives, targeting H. pylori directly is crucial. However, antibiotics alone may not be sufficient because many bacteria are protected by their LPS shield. While the standard H. pylori treatment seeks to use a method to reduce the stomach acids with substance such as (Omeprazole belongs to a class of drugs known as proton pump inhibitors (PPIs)) – hopefully they do this short terms only. They dont seem to target the LPS itself and hence you have reoccurance of the H. Pylori, largely becuase in many cases, the antibiotic killed only those bacteria that were exposed outside of the shell (LPS).
Bacteria seem to become resistant to the antibiotics.
- Those bacteria within their little “LPS Bubble” are protected from immue response, antibiotics and they recognise the threat may even build stronger bubbles for the next attack. Medical professional will note that on second treatment,thing just dont work.. and they say to their collegule. ” These bacteria build up resistance to the treatment” .. it is not that the bacteria is or has become resisitant, it is that they have gone into protective mode and built out a better matrix using LPS, and hance no immune response or antibiotic can get to them. This can also lead to the patient becoming worst, becuase the bacteria may start to dig deeper into the linging of the small intesting or Stomach to protect itself… hence more “leaky gut”.
Thing LPS breakdown along with your strategy!
- Breaking Down LPS: Using substances that can disrupt the LPS shield will enhance the effectiveness of antibiotics. Consider the following:
- Chitosan: Known for its ability to strengthen the gut barrier, reduce inflammation, and have antioxidant properties. It can bind to LPS and help in breaking down this protective layer.
- Activated Charcoal: Highly effective at adsorbing toxins, including LPS. It can prevent the absorption of LPS into the bloodstream, reducing systemic inflammation.
- Zeolite Clay: Has a high cation exchange capacity and can bind to various toxins, including LPS, indirectly reducing their harmful effects.
- Bentonite Clay: Swells and absorbs toxins, helping to remove LPS and other impurities from the gut
- NAC (N-acetylcysteine) is one of the most effective methods, according to research, for breaking down LPS (lipopolysaccharides). Additionally, it is an amino acid that supports the liver in producing glutathione, a powerful antioxidant essential for detoxification and overall health. ( Click Here to get thee 600mg format with Selinium included)
- Mastic Gum is an effective binder with lower side effect on the binding of our minerials.
- Supporting Gut Health: Maintaining a healthy gut microbiota and enhancing gut barrier function are crucial. Probiotics can help restore the balance of beneficial bacteria and prevent the translocation of LPS from the gut into the bloodstream. ( Video the video here)
- https://youtu.be/nMdyFkOBZgc?si=6GM_fveI78v1c8w4
- Dietary Adjustments: Eating a diet rich in fiber, fermented foods, and antioxidants supports gut health and reduces inflammation. ( Because these are Plants – they should be you “DAY TIME FOOD”). Your evening meal must be ( MEATS : Fish, eggs, beef, chicken/Turkey, goat, lamb, others -Rumanints animals. Eat these meats by them selves, and ensure that when you eat, you add Betain HCL to add acid to your stomach to digest the meat into Amino Acids.

By integrating these strategies, you can disrupt the bacteria’s protective mechanisms and enhance the effectiveness of antibiotics, ultimately breaking the vicious cycle of LPS-induced inflammation and gut damage. This comprehensive approach can help restore your gut health and prevent further complications./
Protocol:
Get your GP or Doctor to reveiw this article and he or she may just compliment your standard H. Pylori or other such viral toxins treatment with this recommendations. Even with antifungal load, we need to break the bioflim while we treat the infection. ( I wish i knew these things before now).
A GP with good background in the inner working of these gram negative bacteria will immidately take a progressive note and find the knowledge – he may include Chitosan and cheap suppliment that you can find on amazon.com
Remember it is also your awareness that you need to understand when you are killing and breaking down these houses, they will need to be carries away, hance zeolite or activated chalkcold to bind these toxic waste for dumping in the poo.
N-acetylcysteine (NAC) and chitosan have both been studied for their potential to disrupt biofilms, including those formed by Candida albicans.
N-acetylcysteine (NAC)
NAC is an antioxidant that has shown promise in disrupting biofilms due to its ability to:
- Reduce Extracellular Matrix (ECM) Production: NAC can reduce the production of extracellular polysaccharides that are crucial for the biofilm structure.
- Disrupt Biofilm Architecture: NAC can break down the established biofilm matrix, making the cells more susceptible to antifungal agents.
- Antioxidant Properties: By reducing oxidative stress, NAC can alter the environment within the biofilm, making it less conducive for biofilm maintenance.
Chitosan
Chitosan, a natural polysaccharide derived from chitin, has been shown to have antimicrobial and antibiofilm properties:
- Disrupt Biofilm Integrity: Chitosan can disrupt the structural integrity of biofilms by interfering with the cell wall and membrane of microbial cells.
- Inhibit Biofilm Formation: Chitosan can prevent the initial adhesion of cells to surfaces, thereby inhibiting biofilm formation.
- Enhanced Penetration: Chitosan can enhance the penetration of antifungal agents into biofilms, increasing their efficacy.
Combined Use of NAC and Chitosan
Combining NAC and chitosan could potentially offer a synergistic effect in breaking down biofilms. NAC can disrupt the biofilm matrix and reduce oxidative stress, while chitosan can directly disrupt cell membranes and enhance the penetration of antifungal agents. This combination could be more effective than either agent alone.
Practical Considerations
- Dosage and Delivery: The effectiveness of NAC and chitosan depends on the appropriate dosage and method of delivery. For example, topical application or incorporation into antifungal treatments might be necessary.
- Synergy with Antifungal Agents: Both NAC and chitosan can enhance the efficacy of conventional antifungal treatments, potentially reducing the required dosage and minimizing side effects.
Research and Evidence
While there is promising evidence from in vitro studies and some clinical research, more extensive clinical trials are needed to establish the optimal use of NAC and chitosan for biofilm disruption in Candida albicans infections.
Overall, NAC and chitosan are promising agents for the disruption of Candida albicans biofilms, potentially improving the outcomes of antifungal treatments.

Great videos for LPS here: