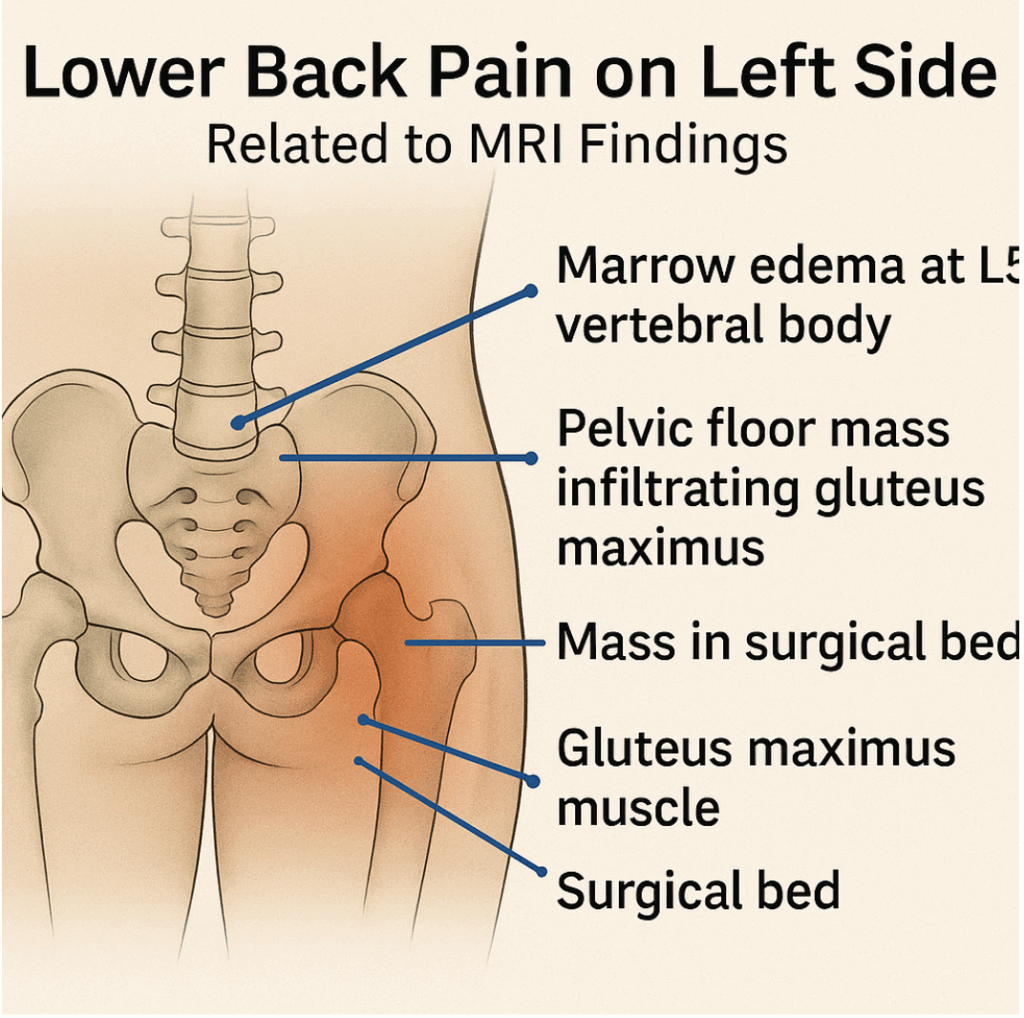
This image highlights key anatomical regions affected by recurrent rectal cancer as identified on the MRI pelvis report dated May 13, 2025, in patient Imi Chitterman. The following findings correlate with the patient’s reported left-sided lower back and pelvic pain:
- Marrow Edema at L5 Vertebral Body
- Identified as abnormal signal intensity in the right anterior lateral aspect of the L5 vertebra.
- Concern: Possible bone metastasis.
- Impact: May cause referred or generalized pain across the lower back, including the left side due to neural and structural interconnection.
- Pelvic Floor Mass Infiltrating Gluteus Maximus
- The tumor mass shows extension into both gluteus maximus muscles, more prominent on the left side.
- Impact: Causes deep tissue inflammation, stiffness, and pain radiating to the lower back and buttock area.
- Mass in Surgical Bed (Pelvic Floor)
- A recurrent mass (~5.2 x 5.3 cm) is located in the region of previous AP resection, involving pre-sacral fat and pelvic floor tissues.
- Impact: This mass increases pressure on nerves and lymphatic vessels, contributing to chronic pelvic pain and muscular tension.
- Bladder Wall and Lymph Node Involvement (not shown in image)
- The mass also touches the left posterior bladder base, with confirmed metastatic lymph node in the left groin.
- These findings, though not directly visible in the image, contribute to pelvic organ dysfunction and lymphatic blockage, indirectly amplifying lower back discomfort.
This illustration serves to visualize the connection between structural MRI findings and the functional symptoms experienced by the patient, especially chronic left lower back pain, pelvic tightness, and muscle inflammation. It underscores the need for integrative therapy, including targeted lymphatic and inflammation support while systemic treatment is being scheduled.
To increase the effectiveness of chemotherapy like Irinotecan, especially in your case of recurrent rectal adenocarcinoma with kidney/bladder vulnerability and immune modulation strategies already in place, here’s a precision support strategy structured for before, during, and after chemo.
CHEMOTHERAPY SUCCESS STRATEGY (HOLISTIC & EVIDENCE-ALIGNED)
1. BEFORE CHEMO STARTS: Prime the Terrain (2–14 days prior)
| Focus Area | Key Actions |
|---|---|
| Immune & Mitochondria Prep | – Take CoQ10 (100–200 mg) + alpha-lipoic acid + NAC to prime antioxidant defense. – Add glutamine (5g/day) to protect mucosal barrier. |
| Hydration & Drainage | – Drink at least 2–2.5L/day with minerals (potassium citrate, sea salt). – Castor oil packs, vibration therapy, or lymphatic massage. |
| Alkaline Cell Support | – Include leafy greens, lemon water, small doses of malic acid or ACV to help shift intracellular pH. |
| Inflammation Control | – Continue taurine, glycine, magnesium, serrapeptase — reduce biofilm and fibrosis. |
2. DAY OF CHEMO: Enhance Delivery, Protect Organs
| Timing | Action Plan |
|---|---|
| Morning | – Light protein-fat meal (eggs + avocado or fish + olive oil) – Take curcumin, omega-3s (fish oil), and CoQ10 for mitochondrial protection. – Hydrogen gas therapy: 30–60 minutes pre-chemo. |
| During Infusion | – Consider Rife frequency or binaural tones to promote parasympathetic state. – Stay warm, calm, and hydrated. |
| Evening | – Avoid sugar or heavy meals. – Take glutamine, probiotics, and herbal teas (like ginger or slippery elm) to protect gut. |
3. BETWEEN CHEMO CYCLES: Regenerate and Repair
| Goal | Support Tools |
|---|---|
| Liver Support | – Use milk thistle, artichoke extract, or dandelion tea. |
| Bladder + Kidney Protection | – Stay on coconut water + potassium, continue taurine + shilajit. – Urinalysis weekly if possible. |
| Mitochondrial Restoration | – Niacinamide (250 mg), PQQ, and L-carnitine if tolerated. |
| Nervous System & Fatigue | – Magnesium glycinate, ashwagandha (if no immune contraindication). |
| Tumor Microenvironment | – Use red light therapy, low-dose melatonin (1–3 mg) at night for immune signaling. |
4. LAB & SYMPTOM MONITORING
| Track Weekly or Biweekly | Goal |
|---|---|
| CRP, LDH, ESR | Should trend downward or remain stable. |
| Creatinine, GFR | Remain within healthy range; GFR ideally trending to >90. |
| CEA | Tumor marker: Stable or decreasing = positive response. |
| Urine Output | Steady volume, no pain, clear → catheter flow healthy. |
| Energy, Pain, Weight, Mental Clarity | All improving or stable between infusions is a good sign. |
5. DON’Ts DURING CHEMO
- Avoid high-sugar foods, refined carbs → they feed inflammation and possibly cancer cells.
- Don’t fast without supervision — fasting may help in some contexts, but you must not lose muscle.
- Avoid high-dose antioxidants DURING chemo infusion — they may blunt the oxidative effect Irinotecan needs to kill cancer cells. Space them out (take at night or next day).
What You Can Do If Irinotecan Is Prescribed
| Action | Purpose |
|---|---|
| Start gentle gut protection (glutamine, probiotics) | Prevent mucositis, support barrier function |
| Monitor hydration and electrolyte levels | Prevent chemo-induced dehydration |
| Ask about support meds: loperamide, atropine | To manage diarrhea risks |
| Track urine and bladder output daily | Protect kidney-bladder pathway |
| Ask for dose-adjustment review | If kidney markers are unstable |
Precautions with Irinotecan
- UGT1A1 genetic test may be recommended: Some patients with UGT1A1*28 variant are at higher risk of severe toxicity.
- Kidney and liver function should be closely monitored — critical in your case due to kidney strain and bladder outlet issues.
- Hydration is vital — you must ensure catheterized bladder is draining effectively.
- Avoid grapefruit juice and some herbal products (can interfere with metabolism).
STAGE 1: Restore Drainage, Reduce Pressure, Support Detox
Goal: Open the exits — remove blockages, ease inflammation, restore flow from cells to kidneys to bladder.
1. Maintain Reliable Bladder Drainage
- Continue catheter care to ensure uninterrupted bladder emptying.
- Hydration: Small, steady intake of clean, mineral-balanced water (e.g., coconut water + sea salt or potassium citrate mix).
- Avoid holding urine or delayed drainage.
2. Support Lymphatic and Interstitial Flow
- Gentle lymphatic massage around groin, abdomen, lower back.
- Castor oil packs over lower abdomen and flank for 45–60 min daily.
- Rebounder (if strong enough) or gentle vibration therapy to activate lymph.
- Herbal support:
- Red clover, cleavers, dandelion root (lymph + liver).
- Parsley, horsetail, corn silk (urinary diuretics), cleavers.
Avoid anything that causes sharp detox reactions until bowel, kidney, and bladder pathways are reliably open.
3. Reduce Inflammation and Biofilm Load
- Continue glycine + collagen for tissue repair.
- Add serrapeptase or SerraDefend or Interface Plus (you’ve used it before) to break down scar tissue and biofilm.
- Include curcumin, taurine, magnesium, and shilajit — for calming inflammation, mitochondrial support, and intracellular flow.
STAGE 2: Restore Kidney Microcirculation and Filtration
Goal: Protect nephrons, improve mitochondrial energy, and reduce acid waste burden.
1. Alkalize Cell Environment Carefully
- Continue potassium citrate (good choice for alkalinity + stone prevention).
- Consider malic acid from apple cider vinegar or tart apple, especially to soften stones or sludge.
2. Protect and Energize Kidney Cells
- Amino acids: Especially glycine, taurine, arginine (improve filtration).
- Mitochondrial support: CoQ10, alpha-lipoic acid, methylene blue (low dose), NAD+ or niacinamide.
- Avoid overuse of high-phosphorus or oxalate foods until kidney filtration improves. NO RAW VEGS !
STAGE 3: Rebuild Immunity + Monitor Cancer Progression
Goal: Strengthen immune surveillance and avoid recurrence triggers.
1. Pro-resolving lipid mediators (SPMs)
- Found in high-quality fish oil or from resolvins (EPA/DHA-derived) — reduces chronic inflammation without suppressing immune system.
2. Immune Modulation
- Mushrooms (reishi, turkey tail, lion’s mane) — support immunity without overstimulation.
- Zinc + selenium — protect DNA and boost T-cell function.
- Low-dose naltrexone (LDN) — consider asking doctor if suitable (immune regulation, anti-cancer effects).
3. Test & Track
- Request regular eGFR, creatinine, CRP, and LDH labs.
- Re-evaluate PSA, CEA, and MRI/CT within oncologist’s guidance.
